
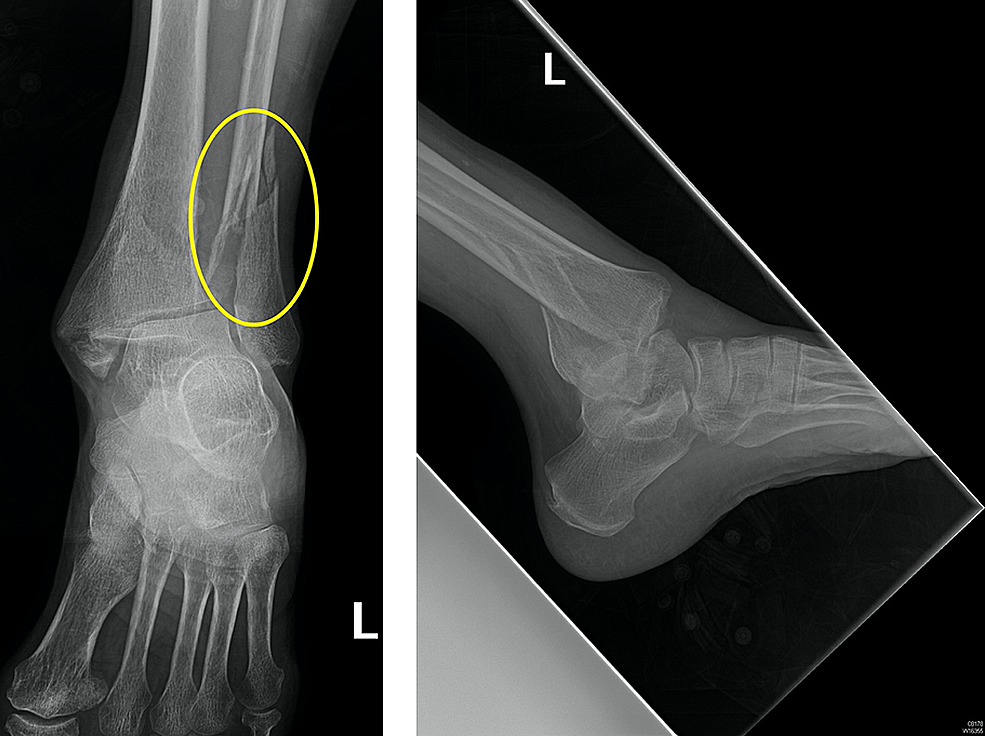
They can show where the bones are broken and if any of the bones are out of place (displaced). X-rays provide images of dense structures such as bone. X-rays. Most ankle fractures can be diagnosed with X-rays. If your doctor suspects an ankle fracture, they will order one or more of the following imaging tests to diagnose and evaluate the fracture (Simanski CJ, JOT 2006 20:108).After discussing your medical history and how the injury occurred, your doctor will do a careful examination of your ankle, lower leg, and foot. 100% good results Olerud score (90 +/- 13 points).
Trimalleolar fx full#
Post-op: bulky jones dressing, NWB, elevation.We discussed the risks of surgery including, but not limited to: incomplete relief of pain, incomplete return of function, nonunion, malnunion, painful hardware, hardware failure, compartment syndrome, CRPS, DVT/PE and the risks of anesthesia including heart attack, stroke and death.Peroneal tendon pathology: associated with low plate placement with a prominent screw head in the distal hole.Lateral malleolar fixation provided with posterior antiglide plate +/- lag screws.document osteochondral injuries which should be saught during ORIF.Prep and drape in standard sterile fashion.Well-padded tourniquet placed high on the thigh.Supine position with bump under ipsilateral hip.Pre-operative antibiotics, +/- regional block.FHL is medial and protects posterior tibial artery/nerve. Find interval between FHL and peroneal tendons. Incision between Achilles and peroneal tendons.

Posterior approach only needed for large posterior malleolar fragments-prone position.Posterior malleolar fragments >25% of the plafond may be fixed via percutaneous clamp reduction through the medical mallellar fracture or direct reduction through a posterolateral or posteromedial approach.
Trimalleolar fx skin#
Delayed surgery done when blisters have resolved, skin wrinkles normally (average 14 days) has equivalent outcomes (Karges/Watson, JOT 1995 9:377). Ideally surgery is done before any true swelling or fracture blisters have developed.


 0 kommentar(er)
0 kommentar(er)
